The connection between obesity and Obstructive Sleep Apnea
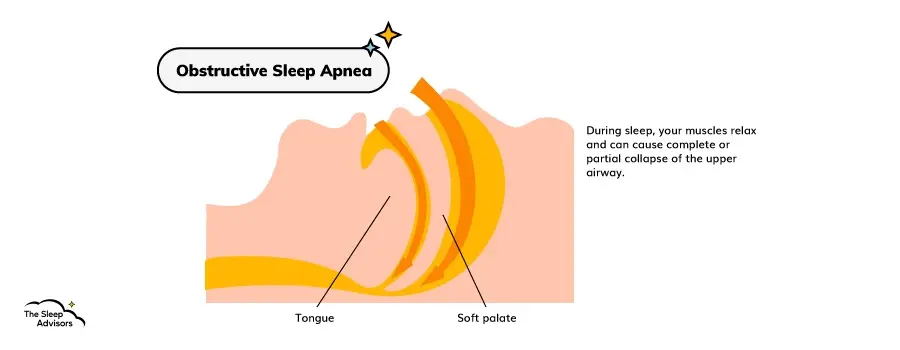
To understand why this new study might change the way physicians approach treatment for severe sleep apnea, we have to establish how obesity and OSA are connected. Generally, Obstructive Sleep Apnea is caused when an individual's tongue or soft palate creates a partial or complete blockage in their airway.
This is most common during the night, which is why OSA is classified among sleep disorders and can lead to worse sleep quality. And the severity of sleep apnea is measured by the number of times your airway is obstructed. This is a measurement called an apnea-hypopnea index (AHI), which will come up later in the article.
But how is your weight connected to any of this?
Well, since Obstructive Sleep Apnea occurs in your throat, fatty tissue around your tongue and soft palate can make it easier for your upper airway to get blocked. On top of that, substantial fatty tissue around your stomach can hamper your breathing and exacerbate the problem.
This is especially common in men who sleep on their backs. However, it's worth noting that while obesity and diabetes are risk factors for Obstructive Sleep Apnea, this relationship is not completely understood. In fact, an obese individual could have a robust upper airway dilator muscle and not experience Obstructive Sleep Apnea at all.
What is wrong with CPAP therapy?
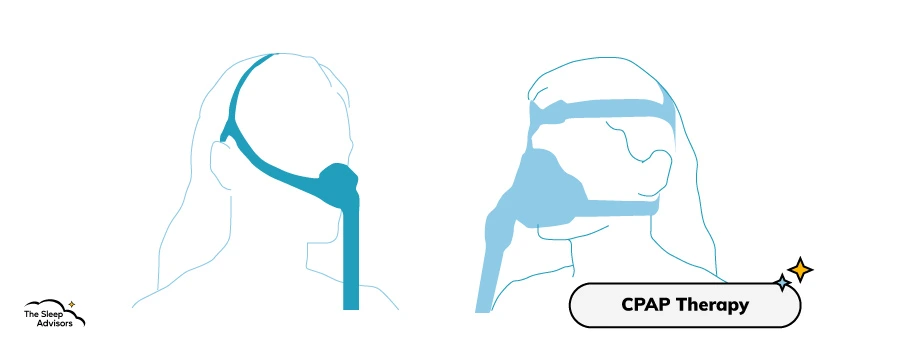
CPAP stands for continuous positive airway pressure and it's one of the most common ways to deal with Obstructive Sleep Apnea symptoms. The way it works is that it “pumps” positive airway pressure through your nose and/or mouth, opening up your airway and lowering your AHI.
It's used to treat severe and mild sleep apnea, and it deals with central sleep apnea as well as Obstructive Sleep Apnea. To keep things short, Central Sleep Apnea is very similar to OSA, usually differentiated due to a “lack of drive to breathe” when an obstruction does happen.
Regardless, when it comes to sleep-disordered breathing, positive airway pressure seems to get the job done. However, if this was the perfect way to have Obstructive Sleep Apnea treated, we wouldn't be here. So, let's quickly mention some issues people who use a CPAP machine might experience.
Difficulties falling asleep
People who want to treat Obstructive Sleep Apnea often want to do so due to the daytime sleepiness and insomnia this condition causes (along with other potential issues). However, wearing a CPAP machine can make it just as difficult to fall asleep.
For one, depending on the type, CPAP machines can be quite bulky, which can cause some people to feel claustrophobic. Plus, side sleepers will have to get used to sleeping on their backs to keep the mask on properly. And if you only have moderate sleep apnea, this could cause more harm than good when it comes to falling asleep.
Plus, while the sound of the CPAP machine could become relaxing over time, it's not a white noise machine, so, people might find it annoying at first.
Potential irritation
While this can vary from person to person and depends on the type of CPAP mask you use, some people might experience slight irritation. To be more precise, they might have nasal congestion, a dry mouth, bloating, and maybe even nosebleeds.
Plus, if you have very sensitive skin, wearing the mask might irritate it as well. And, as we've mentioned, if you can't stop yourself from rolling onto your side, this irritation can worsen.
Convenience
From the excessive daytime sleepiness to the loud snoring, having a sleep-related breathing disorder is already quite inconvenient. However, some people with OSA might find the CPAP itself rather inconvenient as well.
For one, you have to bring it with you when travelling – so, you have a bit less luggage space. And even just storing it in a small room can be a bit annoying.
On top of that, the machine does require maintenance and cleaning. And while some could get the machine for free from NHS, others might have to pay out of pocket. Let's just say that if you want one of the better models, it can cost quite a bit.
Dietary weight loss vs medication vs surgery in OSA sufferers
Now that we've covered all of the background info, let's talk about the actual study at the heart of this article. As we've mentioned, the study set out to see whether weight loss could be the most optimal way to deal with OSA in overweight or obese patients.
So, we're going to go over the numbers they've crunched for the different methods traditionally used to cause weight loss in patients with OSA. And then we'll talk about a specific new medical approach that has so far shown a lot of promise and discuss why it's significant.
Nutrition and exercise

When it comes to weight loss, providing patients with nutritional and fitness education is the least invasive way to solve the problem. As the study notes, this is usually achieved by creating a caloric deficit of at least 500 calories that's then paired with moderate or even intense physical exercise.
In recent times, there have even been more extreme approaches to weight loss. The “very low energy diet” or VLED approach substitutes your regular diet with healthy, low-energy alternatives such as shakes, soups and bars. It then gradually reintroduces higher-energy food into your diet while still staying away from junk food and similar items.
In terms of results, this approach seems very practical in the short term, showcasing as much as a 13.7% weight decrease. However, when it comes to just nutrition and exercise, the results have been mixed when it comes to the long-term effect, with a significant amount of people regaining parts of their weight back over time.
Medication

When it comes to pharmacotherapies, there are a few ways weight loss can be approached. For example, appetite suppressants such as serotonin when combined with diet and exercise can be quite helpful. But things such as phentermine or the lipase inhibitor orlistat have also been used.
By themselves, pharmacotherapies have shown modest results, in the range of 2.8% to 6.1%. But when combined with diet and exercise, this number can go as high as 7.7% of one's total body weight.
This covers some of the traditional approaches to pharmacotherapies when dealing with patients who are overweight and have OSA. However, as we've mentioned, there is a new approach that has shown a lot of promise. We'll cover that as soon as we talk about the final approach to weight loss in patients with Obstructive Sleep Apnea – surgery.
Surgical treatment

When it comes to getting rid of a large amount of excess weight, surgical treatments have shown to be the most effective. Sleeve gastrectomy, gastric bypass and laparoscopic adjustable gastric banding can all be performed to limit cravings and the amount of food people with severe OSA and obesity might consume.
And in terms of results, people have been recorded as losing up to 28% of their overall weight, which is a lot higher than the previous two methods. However, it's important to note that prior to going to the hospital or sleep centre, these procedures do require a strict diet. So, part of the weight loss should be attributed to that.
That being said, procedures like Roux-en-Y gastric bypass (RYGB) have shown to be somewhat consistent in the long run. One study notes that after 12 years, 93% of patients who underwent the procedure were at least 10% lighter than when they started.
However, surgeries are the most invasive procedure and can be difficult to actualise for some people. This is why an alternative method would be ideal for many.
A new approach to OSA treatment via weight loss
So, what's this new weight loss practice? Well, it has to do with Glucagon-like peptide 1 (GLP-1). It's a gastrointestinal peptide that largely deals with food intake and the breaking down of glucose. Naturally, it only has a shelf life of a few minutes. However, synthetic peptides have been created (GLP-1 receptor agonists – GLP-1RA) that can stay in the body much longer.
There are two main variations of these agents that have been tested so far. They are Liraglutide and Semaglutide. The former has shown weight loss of 8% without additional efforts, which is actually quite impressive. However, it's a daily injectible, which can be a problem for some people.
The latter, however, can last up to 180 hours, making it a lot more practical. On top of that, a 35% decrease was observed in a laboratory-meal study. However, a much more realistic number is the one recorded in the Semaglutide Treatment Effect in People (STEP) study, where about 15-16% weight loss was observed.
The issue with this treatment
While this new approach is definitely promising, it's important to note that there have been bumps in the road as well. For one, as we've mentioned, injectibles aren't going to be for everyone and getting hold of them can prove to be just as difficult.
Secondly, slight side effects have been observed – mostly dealing with gastrointestinal issues. And while only a small number of participants opted out of the study due to these issues, they're still worth mentioning.
Lastly, in the STEP study, it has been observed that many of the participants have regained some of their weight. And since continuous treatment could lead to a dependency of sorts, researchers have to find the interval at which these pharmacotherapies can be taken safely.
What this means for people with Obstructive Sleep Apnea
So, what does any of this actually mean for people with Obstructive Sleep Apnea? Well, for the time being, it just means that more options might become available in the near future.
For one, this new research won't help everyone with OSA. As we've mentioned, obesity is closely tied to Sleep Apneas but it isn't the same thing. In other words, even if Semaglutide was perfected and mass-produced, not everyone with OSA would stand to benefit.
On the other hand, if your OSA is tied to your weight, this is a great sign for things to come. After all, medication is less invasive than surgery, is usually easier to get hold of, and can apparently offer better results. Plus, if the treatment is perfected, you should be able to keep excess weight off and massively improve your quality of life.
How is Obstructive Sleep Apnea diagnosed?

When it comes to diagnosing Obstructive Sleep Apnea, there are quite a few ways to go about it. And having it diagnosed can be very important since apneas can sometimes just sound like loud snoring. So, if you get an anti-snoring pillow, you'll be in for a rude awakening when the apneas persist.
Plus, OSA can be an indicator of other medical issues or even cause other problems. The most common way this comes about is when your OSA causes poor sleep quality and the ensuing insomnia starts causing other issues.
So, to diagnose Obstructive Sleep Apnea, you'd typically want to go to a sleep clinic for a physical exam or overnight sleep study. There, they can determine whether you have OSA via a few tests.
They might do so by tracking the number of apneas you have in one hour (or the AHI), with anything over 5 episodes per hour being considered mild or severe sleep apnea. They can also be more thorough and perform the respiratory-disturbance index (RDI), which also takes note of how many times your apnea wakes you up.
Can you diagnose yourself with OSA?
If going to a sleep clinic seems a bit too intimidating, there are other options. Namely, there are a few Obstructive Sleep Apnea tests that you can take from the comfort of your home. For example, you can get one from CPAP or Sleep Test but there are other options as well.
Generally, these services will put you in contact with a doctor through whom you'll get the necessary equipment and an analysis once the test is done. These types of tests are usually priced at around 200 pounds, so, depending on your insurance, they could be more or less expensive than a regular visit.
However, it's important to note that these types of trackers can't always pick up on other sleep disorders and/or problems. So, if there's more going on than just OSA, you'll likely need a sleep clinic to get the full picture.
Lastly, when it comes to regular sleep trackers, we wouldn't recommend leaning on them. Higher-end models can let you know if you've woken up during the night but that could be caused by a number of different problems. Likewise, we also wouldn't recommend diagnosing yourself by recording yourself at night or having your partner do it.
Obstructive Sleep Apnea can just sound like snoring to some and it can be difficult to determine how high the AHI is or how intense the apneas are. So, regardless of how you go about it, a doctor should be involved.
Other factors that influence Obstructive Sleep Apnea Syndrome
While excess weight is a major risk factor for Obstructive Sleep Apnea, it's not the only one. So, to give you a clearer picture of what else can cause this sleep disorder, we'll quickly list some of the other risk factors.
- OSA is more common in men than in women
- OSA is more common in older individuals
- OSA is tied to a high blood pressure (hypertension)
- OSA is common in smokers and people with asthma
- A narrowed airway or chronic nasal congestion can also cause OSA
- If someone in your family has a medical history with OSA, you're more likely to have it as well
And remember, if you're just experiencing daytime sleepiness, it doesn't have to be OSA that's causing it. Anything from Seasonal Affective Disorder to insomnia can cause this effect.
Alternatives to CPAP therapy
If you have Obstructive Sleep Apnea but don't want a CPAP machine and you don't have any issues with your weight, what other options are there? Well, while they might not be as effective, for treating mild OSA, you do have a couple of other options.
- Positional therapy – This just means avoiding sleeping on your back, since it often triggers Obstructive Sleep Apnea.
- Oral appliance therapy – This means having a sort of teeth guard made that can help keep your jaw in a better position.
- Surgery – While we've already mentioned how surgery can aid in weight loss and thus help deal with Obstructive Sleep Apnea, there are procedures for dealing with the issue directly. This is usually done in severe cases and can target your soft tissue or the jaw.
Overall, there aren't too many alternatives out there. However, it's important to know all of your options.
Conclusion
In conclusion, there are a few ways you can deal with Obstructive Sleep Apnea. It can be as simple as rolling over in bed or as complex as getting surgery. However, in the long run, weight loss should be considered for many.
And with the continued research in the field of pharmacotherapies, treating Obstructive Sleep Apnea through weight loss might become the go-to option for some patients. However, we do implore you to read the full study that has been the basis of some of our claims, as we had to leave a lot of information out.
And if you have any questions, feel free to ask us in the comments – especially if you also have Obstructive Sleep Apnea.










There are no comments yet
"*" indicates required fields